Cornea transplant cost and its importance
A cornea transplant is a surgical procedure which replaces a damaged or diseased cornea with a healthy donor cornea. The cornea is the eye’s clear, dome-shaped front surface that plays a crucial role in focusing vision. Corneal transplants are performed to restore vision, reduce pain, and improve the appearance of a damaged or diseased cornea.
Cornea
The cornea is the eye’s outermost transparent layer of the eyeball which plays pivotal role to bend the light rays to converge at the cornea. The normal average power of each cornea is 43D. The cornea is generally described as having an elliptical shape when viewed from the front. However, its curvature is not uniform. The central part of the cornea is steeper, while the peripheral parts are flatter.
Dimensions of cornea
The average horizontal diameter of the cornea is about 11.5 to 12.0 millimeters (mm). The vertical diameter is slightly smaller, averaging around 10.5 to 11.0 mm. At the center (the thinnest part), it measures approximately 540 to 550 micrometers (µm), while the peripheral cornea is thicker, measuring around 600 to 700 µm.
Criteria for cornea transplant
Not everyone with corneal issues is a candidate for a transplant. Specific criteria must be met to be considered for the procedure:
Corneal dystrophies and degenerations
Conditions such as keratoconus, Fuchs’ dystrophy, corneal scarring from infections or injuries, and hereditary corneal conditions may necessitate a transplant.
Significant vision loss due to cornea
When vision is significantly impaired and cannot be corrected with glasses, contact lenses, or less invasive surgeries, a corneal transplant may be recommended
Infections due to contact lens
The excessive wearing of contact lenses and not letting the natural cornea to breathe let it to develop severe bacterial infections leading to pain and opacity which in turn leads to corneal transplants.
Opacity
Patients with a severely thinned or opaque cornea that affects vision might be eligible for a transplant.
Unsuccessful corneal surgeries
Individuals who have had unsuccessful corneal surgeries in the past may require a transplant.
Progessive corneal degenerations
While there is no strict age limit, younger patients with progressive conditions like keratoconus might benefit more from an early transplant.
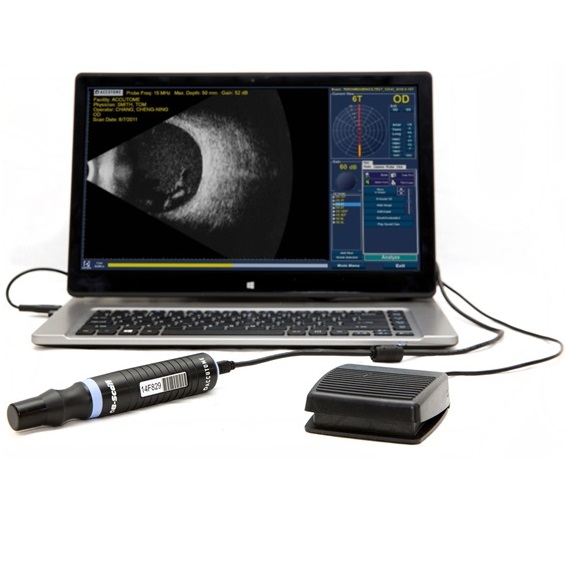
Basic assessment criteria
Before the surgery, a thorough eye examination is conducted to determine the extent of corneal damage and assess overall eye health. The patient’s medical history is reviewed, and measurements of the eye, such as corneal thickness and curvature, are taken to ensure the best possible match.
Transplant surgery
On the day of the surgery, local or general anesthesia is administered to ensure the patient’s comfort. Local anesthesia involves numbing the eye with drops or injections, while general anesthesia puts the patient to sleep. This surgery doesnot take more than an hour.
The eye and surrounding area are cleaned with an antiseptic solution to prevent infection.
A circular cutting device called a trephine is used to remove the damaged portion of the cornea. The size of the removed cornea is carefully measured to match the donor tissue.
The surgeon removes the central part of the cornea, creating a circular opening for the donor cornea.
Donor cornea
The donor cornea is prepared by cutting it to the appropriate size using a trephine. The quality and health of the donor tissue are checked to ensure suitability.
The donor cornea is then placed into the opening created in the patient’s cornea. The graft must be positioned precisely to ensure proper alignment and function.
The donor cornea is then placed into the opening created in the patient’s cornea. The graft must be positioned precisely to ensure proper alignment and function.
Tiny, delicate stitches (sutures) are used to secure the donor cornea in place. These sutures help the cornea heal properly and maintain its shape.
Aftercare
After the surgery, an eye shield is placed over the eye to protect it from injury and infection.
Taking prescribed medications
The patient is prescribed antibiotics and anti-inflammatory eye drops to prevent infection and reduce swelling.
Follow-ups
Regular follow-up visits are scheduled to monitor the healing process and manage any complications if needed.
Vision stabilization
Vision gradually improves as the eye heals, though full visual recovery can take from months to a year.
Regular check-ups
Continued use of prescribed eye drops and regular check-ups with the ophthalmologist are advised.
How to start cornea tranplant
The journey to a corneal transplant begins with an initial consultation with an ophthalmologist including complete eye examination, history review and mandatory diagnostic tests.
Who is the actual reciever
Not everyone with corneal damage is a candidate for a transplant. The ophthalmologist will consider severity of the corneal damage and previous history. History of unsuccessful corneal surgeries may indicate the need for a transplant.
Process
Once if someone is identified as a candidate for cornea transplant then he or she is put on the waiting list and he is either registered for the eye bank’s waiting list or referred to the eye bank and the procedure is explained to the person through his eyecare practitioner.
How to find the donor
Once you are declared a potential candidate for cornea transplant, the next step is finding a suitable donor corneaThe donor cornea is matched based on tissue compatibility.
Average cost
The average cornea transplant cost can vary upon zero to 10,000 USD or even more. Surely their are donations or aids for someone who can not afford cornea transplant immediately. The full term recovery takes place in 6 months mostly.
Founder of EyesMatterMost- an optometry student who loves talking about eyes. I tend to cover topics related to optometry, ophthalmology, eye health, eyecare, eye cosmetics and everything in between. This website is a medium to educate my readers everything related to eyes.