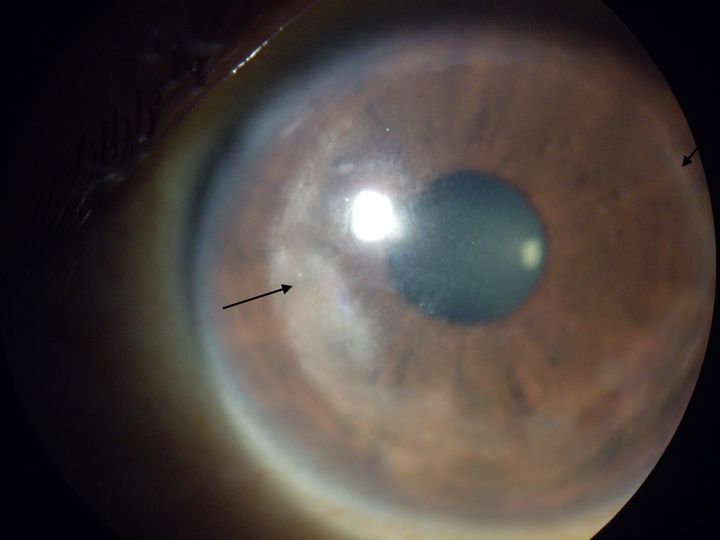
Corneal haze- causes, symptoms, treatment and prevention
Corneal haze, also known as corneal opacity, is a condition that affects the transparent outermost layer of the eye, the cornea. This condition can have a significant impact on a person’s vision specifically when haze is present at the center of the cornea.
Compromising the transparency
The cornea is the clear, dome-shaped surface at the front of the eye that plays a crucial role in focusing light onto the retina. It is essential for clear vision. When the cornea becomes cloudy or hazy, it can interfere with the passage of light, leading to a reduction in vision quality. It is the result of a disturbance in the cornea’s structure, which scatters light and reduces its transparency.
Causes
It can be caused by various factors, including:
Infections
Bacterial, viral, or fungal infections of the cornea can lead to inflammation and scarring, resulting in corneal haze.
Ocular trauma
Trauma or injury to the cornea, such as from a foreign object or a chemical burn, can cause corneal haze
Surgeries
Certain eye surgeries, such as LASIK (Laser-Assisted In Situ Keratomileusis) or photorefractive keratectomy (PRK), can result in temporary corneal haze as part of the healing process.
Pterygium
A pterygium is a growth of tissue on the cornea, and it can lead to this condition if left untreated.
Corneal dystrophies
Inherited conditions that affect the cornea, such as Fuchs’ dystrophy, can lead to corneal haze over time.
Symptoms for corneal haze
- Blurred or hazy vision
- Glare or sensitivity to light
- Halos around lights
- Reduced night vision
- Eye pain or discomfort
- Foreign body sensation in the eye
Diagnosis
Diagnosing corneal haze typically involves the following:
Visual acuity test
This measures your ability to see clearly and is usually the first step in evaluating vision problem.
Slit lamp examination
A slit-lamp microscope allows the ophthalmologist to closely examine the cornea for signs of haze, scarring, or other abnormalities
Corneal topography
This technique creates a detailed map of the cornea’s surface, helping to identify irregularities in its shape.
Specular microscopy
This test assesses the health and density of corneal endothelial cells, which are critical for maintaining corneal clarity
Pachymetry
It measures the corneal thickness is important, especially if it’s related to corneal dystrophies or eye surgeries.
Treatment
Medications
If the corneal haze is due to infection or inflammation, topical or oral medications may be prescribed to control the condition. These medications can include antibiotics, antifungals, and corticosteroids.
Keratoplasty
In some cases, surgery may be necessary to remove or repair damaged corneal tissue. Procedures like corneal transplant (keratoplasty) can replace the affected cornea with a healthy donor cornea.
Phototherapeutic keratectomy
PTK is a laser-based procedure that removes the superficial layers of the cornea, including the hazy or irregular tissue. It is often used for certain corneal dystrophies.
Corneal cross linking
This procedure is used to strengthen the cornea and slow the progression of conditions like keratoconus, which can lead to corneal haze.
Using contact lenses
Specially designed contact lenses, such as scleral lenses, can help improve vision in some cases of corneal haze by providing a smooth, clear optical surface.
Management
For conditions like keratoconus, managing the underlying condition may help prevent or delay the development of corneal haze.
How to prevent hazy cornea
Wearing safety goggles or protective eyewear when engaging in activities that could pose a risk to the eyes while working with chemicals or in sports can reduce the risk of injuries that can produce corneal haze.
It can also be prevented by practicing hygiene and replacement schedules to reduce the risk of eye infections and complications.
Early treatment of any type of eye injury or infection prevents the complications that can lead to this.
Routine eye exams can help detect and manage conditions that may contribute to haze, such as keratoconus or corneal dystrophies.
Prevention through protective measures and regular eye exams is also key to maintaining good eye health and clear vision. If you suspect you have corneal haze or are experiencing any related symptoms, consult with an eye care professional for a thorough evaluation and personalized treatment recommendations.
Founder of EyesMatterMost- an optometry student who loves talking about eyes. I tend to cover topics related to optometry, ophthalmology, eye health, eyecare, eye cosmetics and everything in between. This website is a medium to educate my readers everything related to eyes.