Understanding keratometry- a comprehensive guide
In the world of ophthalmology and vision sciences, precise corneal measurements play a critical role in diagnosing and treating various eye conditions. One such vital measurement is keratometry, a basic test used to measure the curvature of the cornea.

What is keratometry?
Keratometry, also known as corneal topography, is a non-invasive diagnostic procedure to measure the curvature of the cornea’s anterior surface. The cornea, being the transparent front layer of the eye, contributes significantly to the eye’s overall focusing power. It has a refractive power of +44D. By accurately measuring its curvature, ocular physicians can gain valuable insights into a patient’s refractive error, detect astigmatism, and analyze the potential for fitting contact lenses.
The cornea acts as the primary refractive surface of the eye, responsible for bending and focusing light rays as they enter the eye. It is the first and most important part of optical system of the eye as any abnormality in cornea can disturb the bending of light rays. Any irregularities in corneal curvature can lead to refractive errors, such as myopia (nearsightedness), hyperopia (farsightedness), and astigmatism. By obtaining precise keratometry measurements, eye care practitioners can determine the appropriate prescription for corrective lenses or evaluate the candidacy for certain refractive surgeries like LASIK or PRK.
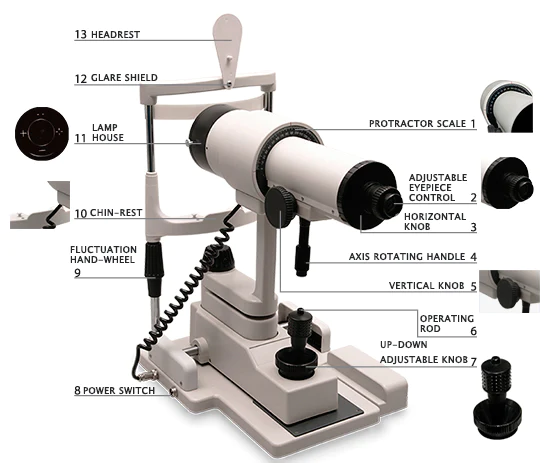
Parts of keratometry
Let us we delve into the essential parts of keratometry and their roles in assessing corneal curvature for enhanced vision.
Chin Rest
The chin rest ensures that the patient’s head remains stable and aligned during the examination. It is adjustable to accommodate different heights and positions, enabling comfortable positioning for the patient.
Viewing System
The viewing system is facing the eye care professional to observe the procedure. In manual keratometry, this system consists of an eyepiece with a target (object) for aligning the instrument with the patient’s eye. In modern corneal topography systems, the viewing system may be replaced with a computer screen displaying the corneal maps and measurements obtained during the tests.
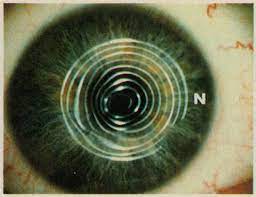
Light source and mires
The light source is a fundamental component in both manual keratometry and corneal topography systems. It is responsible for projecting light rings or patterns onto the cornea. In traditional keratometry, the light source generates concentric rings known as mires. These mires are reflected on the cornea, and the measurements are taken based on their distortion. In corneal topography, different light sources such as placido disc-based or scanning-slit technologies are used to create detailed corneal maps for more comprehensive evaluations. The eye care professional aligns the mires to ensure proper superimposition, allowing for accurate measurements of the corneal curvature along different meridians.
Measuring system
The measuring system in a keratometer is responsible for quantifying the corneal curvature based on the reflections obtained from the mires or light patterns. In manual keratometry, the practitioner manually adjusts the instrument to achieve the desired alignment of mires and then reads the measurements directly from the keratometer’s display.
The Keratometry Procedure
The keratometry procedure typically involves the following steps:
Patient compliance
Before beginning the test, the eye care professional prepares the patient by applying numbing eye drops to ensure comfort during the procedure. The patient is then seated comfortably, and the chin rest is adjusted to stabilize the head.
Alignment
For manual keratometry, the practitioner aligns the instrument with the patient’s eye, ensuring proper fixation on the target.
Measurement
The instrument projects the light rings (mires) onto the cornea. The instrument’s measuring system records the curvature readings (K1 and K2) for the principal meridians.
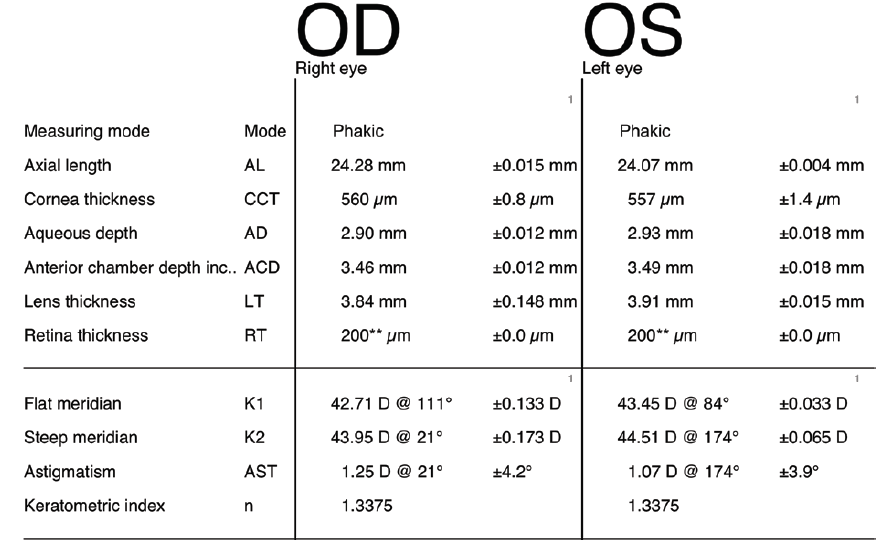
What are K1 and K2 readings?
The keratometry readings are typically expressed in diopters (D). These are presented in two formats, the flattest and steepest curvatures which are represented as K1 and K2 respectively.
Finding refractive errors with K values
If both K1 and K2 readings are within a narrow range or if there is minimal difference between them, it indicates that the cornea has little or no astigmatism, and the refractive error is likely spherical (myopia or hyperopia).
However, if the difference between K1 and K2 readings is significant, it indicates the presence of astigmatism. If K1 is greater than K2, the cornea has with-the-rule astigmatism, which means the steepest meridian is in the horizontal direction. Conversely, if K2 is greater than K1, the cornea has against-the-rule astigmatism, with the steepest meridian in the vertical direction.
Applications of keratometry
Measuring refractive error
One of the primary applications of keratometry is the accurate assessment of refractive errors in the eye. The measurement of curvature of cornea tells the type of refractive error. Based on the difference between K1 and K2 readings, the meatometer calculates the degree and axis of astigmatism. Astigmatism occurs when the cornea has two principal meridians with different curvatures.
Contact lens fitting
Since the cornea is not a perfectly spherical surface, the curvature can vary in different meridians. Keratometry provides measurements of both the flattest (K1) and steepest (K2) curvatures of the cornea, allowing eye care practitioners to select the most appropriate type and curvature of contact lenses for the patient.
Why we need proper fitting of contact lenses
We need proper fitting of contact lenses to enhance comfort and wearibility. Lenses that fit well provide consistent and clear vision across the entire visual field. A well-fitted lens allows adequate tear circulation, which helps maintain the cornea’s health and promotes oxygen supply to the corneal tissues. This reduces the likelihood of corneal complications and ensures the eyes remain healthy and free from irritation or inflammation. Proper fitting of contact lenses prevent lens fitting syndrome which may cause dryness, redness, itching, and a foreign body sensation in the eye.
Pre-operative evaluation for refractive surgeries
Keratometry plays a critical role in the pre-operative evaluation of patients considering refractive surgeries like LASIK (Laser-Assisted In Situ Keratomileusis) or PRK (Photorefractive Keratectomy). These surgeries aim to reshape the corneal surface to correct refractive errors and reduce dependency on glasses or contact lenses. Precise keratometry data enables surgeons to plan the surgery effectively, maximizing the chances of a successful outcome and minimizing potential complications.
Diagnosis and monitoring of corneal diseases
Keratometry is instrumental in diagnosing and monitoring various corneal diseases. One such condition is keratoconus, a progressive disorder that causes the cornea to become thin and bulge into a cone-like shape. By continuously measuring the corneal curvature over time, eye care professionals can identify changes indicative of keratoconus or other corneal irregularities. Early detection allows for timely intervention and appropriate management, helping to preserve vision and prevent further corneal deformities.
Analyzing post-operative outcomes
After undergoing corneal surgeries or certain refractive procedures, such as corneal transplant or intracorneal ring segment insertion, keratometry is essential to assess the post-operative outcomes. These measurements aid in evaluating the cornea’s healing process and identify any irregularities or complications.
Orthokeratology evaluations
Orthokeratology (Ortho-K) is a non-surgical method of temporarily correcting refractive errors (specifically myopia) using specialized gas-permeable contact lenses worn overnight. These lenses gently reshape the cornea, providing clear vision during the day without the need for glasses or contact lenses. Keratometry is crucial in evaluating and monitoring the corneal changes induced by Ortho-K lenses.
IOL power
Keratometry is an important tool used to calculate the power of intraocular lenses (IOLs) for cataract surgery or refractive lens exchange.
Founder of EyesMatterMost- an optometry student who loves talking about eyes. I tend to cover topics related to optometry, ophthalmology, eye health, eyecare, eye cosmetics and everything in between. This website is a medium to educate my readers everything related to eyes.