Stages and classification of diabetic retinopathy
Diabetic retinopathy stages
The diabetic retinopathy is classified on the basis of well-marked photographs described by EDTRS (Early Treatment Diabetic Retinopathy Study).
On the basis of presence or absence of neovascularization, it is divided into two types:
- Proliferative diabetic retinopathy(PDR)
- Non-proliferative diabetic retinopathy (NPDR)
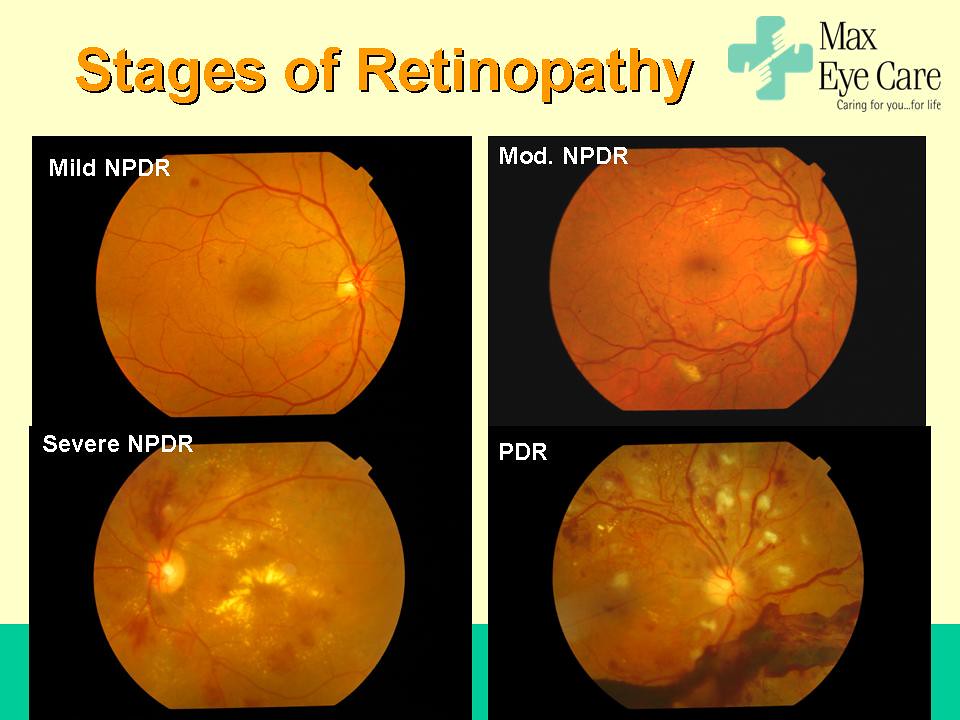
Non-proliferative diabetic retinopathy (NPDR) stages
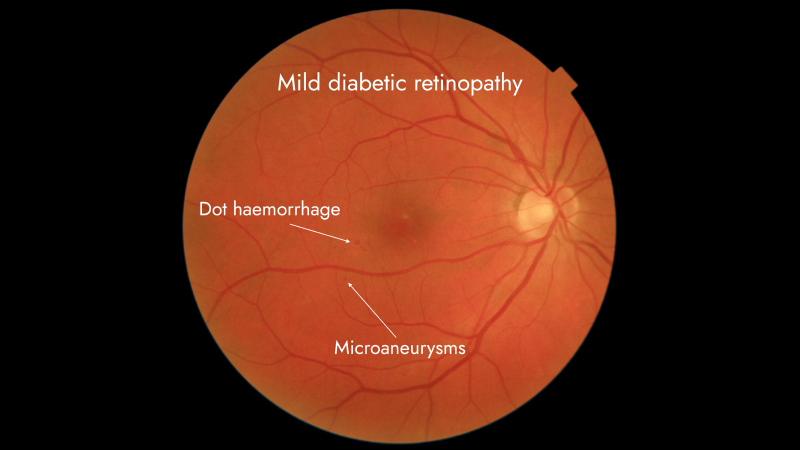
Mild NPDR
In this type, the entire fundus seems normal but there are very small circular spots present. These show indications for micro-aneurysm. This diagnosis is certain when the patients have history of diabetes mellitus. The damaged blood vessels in the retina begin to leak fluids and small amounts of blood into retina.
Moderate NDPR
In this type of diabetic retinopathy, the fundus of patients not only show signs of micro-aneurysms but also dot and blot hemorrhages, cotton wool spots and hard exudates. The blood vessels leak deposits of fats in the blood called hard exudates. The exudates can also be present in the foveal region and the patient can have diabetic macular edema. The damaged blood vessels lose their ability to transport oxygen and nutrients for the nourishment of retina.
Severe NDPR
There is a 4:2:1 rule for the diagnosis of this clinical type of non-proliferative diabetic retinopathy.
- There are internal hemorrhages and micro aneurysms in all the four quadrants in the eye. These quadrants are superior, inferior, nasal and temporal.
- There is venous beading in at least two quadrants. In venous beading there is sausage like dilatation of retinal veins. It is the sign of severe stage of non-proliferative diabetic retinopathy.
- There is intra-retinal microvascular abnormality in at least one quadrant. It is the abnormal dilation, looping or beading of retinal blood vessels triggered by vascular endothelial growth factor which is stimulated by hypoxia in blood vessels. It is the pre-disposition for proliferative stage of diabetic retinopathy. However this can be distinguished from proliferative diabetic retinopathy through a test called fluorescein angiography.
If any of the three things are present then the patient has severe NPDR.
Proliferative diabetic retinopathy
The patients who have severe non proliferative stage of Diabetes are more likely to develop this with in the span of 1 year. When more and more blood vessels are damaged preventing adequate blood flow to retina then it grows new blood vessels for the provision of blood flow. This process is called neovascularization.
These blood vessels are weak, thin and fragile. They often leak into the vitreous. They bleed into vitreous due to their thin and delicate walls causing vitreous hemorrhage. Vitreous is a gel that fills inside of the eye ball from retina to the lens.
The phenomenon of neovascularization occur when minimum of one-fourth of retina is ischemic. Neovascularization can happen on different location in retina.
- Neovascularization on the disc or with in one diameter of the optic disc is called NVD
- New vessels can also arise in retina elsewhere from 1 disc diameter away from the disc and this is called neovascularization elsewhere i.e. NVE
- New vessels occur on the iris due to retinal ischemia called NVI or Rubeosis iridis.
The symptoms for vitreous hemorrhage include
- spots
- scotomas
- reddish tint vision
- It can also lead to vision loss.
The new vessels have fibrotic material which have the tendency to contract and pull retinal layer causing tractional retinal detachment.
Diabetic retinopathy is a common diabetic eye disease which occurs due to changes in retinal cells specifically in those patients who have diabetes for more than 10 years. The regular screening of eye for diabetic patients is very important to prevent these diseases on a large stage.
Diagnosis
Fluorescein angiography
A small amount of yellow dye I injected into arm which circulates through the body vessels and also in retinal vessels. Special cameras with blue flashes are used to take series of pictures of retina and the areas of abnormal leakage, ischemia and hemorrhages become visible.
Optical coherence tomography (OCT)
This diagnostic test helps doctors to get the reason of the blurring of vision to start the required treatment as early as possible.
Treatment
Laser
This type of treatment is a choice when diabetic retinopathy causes macular edema to prevent loss of blood and its components by sealing the leaking blood vessels to restore the proper function of the macula.
For proliferative diabetic retinopathy
For this , there is a laser treatment i.e. Panretinal Photocoagulation (PRP) also known as Scatter Photocoagulation. The target is peripheral retina new vessels to shrink them and prevent them from growing. It decreases the chances of vitreous hemorrhages.
Anti- VEGF injections
These target vascular endothelial growth factors which cause the neovascularization of abnormal blood vessels. An anti- VEGF drug reduces growth of abnormal blood vessels and prevents bleeding and vision loss. After applying anesthesia to the eyes, the anti- VEGF drugs are administered into the eyes with very fine needles. The number of injections varies for patient to patient.
Vitrectomy surgery
This surgical procedure helps in removing vitreous hemorrhage and car tissue. The vitreous is removed and the eye surgeon may place a gas bubble or silicon oil bubble in vitreous space .
Founder of EyesMatterMost- an optometry student who loves talking about eyes. I tend to cover topics related to optometry, ophthalmology, eye health, eyecare, eye cosmetics and everything in between. This website is a medium to educate my readers everything related to eyes.